Abstract
Background:
Immune thrombocytopenia (ITP) usually is a mild and self-limited disease; however, 25-30% of children develop chronic ITP. Nordic score is a validated clinical prediction tool, yet its use in children is limited and evidence for other prognostic factors is unclear.
Purpose:
To evaluate clinical outcomes among pediatric ITP patients, and examine their relationship to patient characteristics, including Nordic score. We hypothesized that Nordic score and patient characteristics will be predictive of ITP resolution or development of chronic ITP.
Methods:
We conducted a retrospective chart review of all children diagnosed with ITP at our institution between May 2008 to May 2019. Data extraction included patients' age, sex, presenting signs and symptoms, laboratory values, treatment decisions, and clinical outcomes. Nordic score calculated with 6 clinical features from diagnosis: abrupt onset <14 days, age < 10 years, preceding infection <1 month, platelet count < 5x10 9/L, wet purpura, and male sex. High scores (10-14) predict a brief disease course (<3 months), whereas low scores (0-4) predict a more prolonged course.
Primary outcomes included complete response (CR) (platelets 100 x10 9/L on 2 occasions >7 days apart), recurrence (platelets < 100 after achieving CR), development of chronic ITP, and resolution (long term normal platelet count). Secondary outcomes included early response (platelets 30 x10 9/L in <1 week), time to CR, duration of CR (months between CR and recurrence), and time to resolution. Data presented as odds ratio (OR) with 95% confidence intervals. OR for Nordic score presented per 5-unit increase correlating with Nordic score categories (low 0-4, moderate 5-9, high 10-14).
Results:
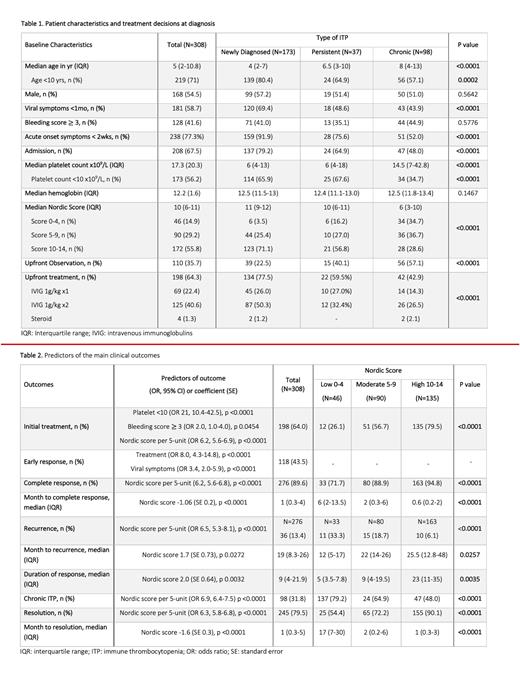
A total of 308 patients were included (median age 5 years, IQR 2.0-10.8; 54.5% male) (Table 1). About 56% presented with platelets < 10 x10 9/L and 42% had bleeding at diagnosis (bleeding score 3 or higher), only 3% were severe. Median Nordic score was 10 (IQR 6-11). Overall, 64% of patients were treated upfront, majority (98%) receiving intravenous immunoglobulin (IVIG).
Treatment at diagnosis was more likely for patients with platelets < 10 x10 9/L (OR 21, 10.4-42.5), bleeding score 3 or higher (OR 2.0, 1-4), and higher Nordic score (OR 6.2, 5.6-6.9) (Table 2). Treatment was predictive only of early response in multivariate analysis, not of CR, recurrence, development of chronic ITP, or disease resolution. Additionally, treatment at diagnosis was not associated with reduction in ITP-related complications, such as major bleeding episodes, need for platelet or red cell transfusions, or iron deficiency anemia.
Overall rate of CR was 90% over a median of 1 month (IQR 0.3-4 months), while 13% had recurrence after median 19 months (IQR 8.3-26.0 months) and 32% developed chronic ITP. Overall, 80% of all study patients had resolution of ITP after median 1 month (IQR 0.3-5), with 86% achieving this before 12 months. About 36% of patients with chronic ITP had disease resolution over median 25 months (IQR 16.3-46.5 months).
Univariate analysis showed significant variation across subgroups for age, viral symptoms, abrupt onset, Nordic score, hospital admission at diagnosis, platelet count, and treatment. Using multivariate regression analysis adjusted for the above variables, Nordic score was the only independent predictor of all primary outcomes. Higher Nordic score group had increased likelihood of CR (OR 6.2, 5.6-6.8) and disease resolution (OR 6.8, 5.1-8.9). Lower Nordic score group was associated with increased likelihood of recurrence (OR 6.5, 5.3-6.9) and development of chronic ITP (OR 8.6, 6.5-11.4). Additionally, higher Nordic score group was associated with increased time to recurrence and duration of response, decreased time to CR and resolution.
Conclusions:
In our cohort, low platelet count and bleeding symptoms were drivers of upfront treatment in pediatric ITP. Treatment initiation, associated with Nordic score, was predictive of faster increase in platelet count; however, it had no impact on overall disease trajectory or likelihood of complications. Our analysis demonstrate that Nordic score is an independent predictor of CR, resolution, recurrence, and development chronic ITP. Nordic score is a useful, simple prognostic tool that has the potential to help predict clinical course of pediatric ITP and identifying patients who may benefit from closer monitoring.
Badawy: Bluebird Bio Inc: Consultancy; Sanofi Genzyme: Consultancy; Vertex Pharmaceuticals Inc: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal